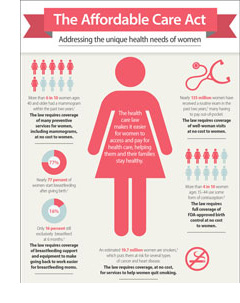
 We hosted a webinar on December 4 -- ACA Basics: Breastfeeding & WIC with Anna Benyo, Senior Health Policy Analyst from the National Women’s Law Center (NWLC). Anna reviewed key components about the Affordable Care Act (ACA) and women's health coverage, specifically coverage of women's preventive health services and the requirement to provide breastfeeding support and supplies.
We hosted a webinar on December 4 -- ACA Basics: Breastfeeding & WIC with Anna Benyo, Senior Health Policy Analyst from the National Women’s Law Center (NWLC). Anna reviewed key components about the Affordable Care Act (ACA) and women's health coverage, specifically coverage of women's preventive health services and the requirement to provide breastfeeding support and supplies.
We also talked discussed ways to be an ACA resource for WIC participants. View the presentation slides.
Here are some Q&A highlights from the webinar. Answers provided by Anna Benyo:
The preventive services provision does not apply to traditional Medicaid, but does apply to Medicaid expansion. That means women in traditional Medicaid don’t have the same coverage as women in Medicaid expansion or in the private market. CMS has said they want to align coverage of the preventive services between traditional Medicaid and Medicaid expansion—so it’s definitely on their radar and part of their goal.
There is also a one percent FMAP increase for states that cover preventive services (those with A and B USPSTF rating) in traditional Medicaid (this does not apply to the women’s preventive health services)
The coverage varies by state. Take a look at these reports for more info on your state by state Medicaid coverage: CMS, Kaiser Family Foundation.
The guidance from HHS is silent on that. They don’t specify whether the provider needs to be a certified lactation consultant or can be a peer counselor, and they also don’t weigh in on reimbursement, see question 19 in the Departments guidance and Frequently Asked Questions (FAQs). It’s up to the insurance company. Each insurance company will decide who to contract with and be part of their network. This is the area where we hear the most complaints—based on feedback we have heard from women trying to access this benefit, they are often not given a list of in-network lactation consultants or told that their insurance company does not have to provide coverage for this service Unfortunately, some insurers do not have adequate lists available. It’s a murky area that’s unclear with many plans and we’re working hard to make sure that people would be able to go online and see a more comprehensive list of lactation consultants.
This is another area where there is some confusion with insurance companies. The guidance from HHS is clear: “Over the counter recommended items and services must be covered without cost-sharing…when prescribed by a health care provider.” Accordingly, insurance companies must cover a breast pump that her and her provider agree will meet her health care needs. So we know that women have to be able to get a breast pump that meets her needs. However insurance companies can use reasonable medical management techniques to determine the “frequency, method, treatment, or setting for a recommended preventive item or service.”
We have heard reports of women who said their insurance company wouldn’t cover an electric pump. It’s important to remember however, that if a provider recommends and prescribes an electric pump, it must be provided without cost-sharing. We know that women have to be able to get a breast pump that meets her needs. Insurers can use reasonable medical management techniques and their documents might say that a manual pump is covered, but when a woman talks to her provider and it’s clear she needs an electric pump or a hospital-grade pump, they would need to call their insurance company and say they need an electric pump and the insurance company must comply. However, insurance companies will want you to go through an in-network Durable Medical Equipment (DME) Company, so it’s not recommended to purchase a pump from a store and ask for reimbursement.
Pregnant and postpartum women have access to comprehensive lactation support and counseling from trained providers, as well as breastfeeding equipment. Coverage extends for the duration of breastfeeding , meaning there is not a set time limit. Coverage is for “comprehensive lactation support and counseling” and “costs of renting or purchasing breastfeeding equipment.”
NWLC is working on a specific breastfeeding-coverage script to talk to your insurer, so that will be shared once it’s completed.
Preventive Services:
Have questions about ACA coverage? Let us know by emailing [email protected] so we can design future webinars to meet your needs!